Meet Breanne Rodgers. Breanne is 21 years old and from Huntsville, Alabama. Recently, she went mega viral on TikTok when she posted a video of her experience trying to get what felt like “constant UTIs” diagnosed and treated. More than a year and multiple doctors later, she was finally able to get an accurate diagnosis — and it wasn’t chronic urinary tract infections at all.
Instead, it was interstitial cystitis — also commonly referred to as “painful bladder syndrome” — which, despite affecting millions of people, can often be dismissed or misdiagnosed.
In the video posted to her TikTok account — which has since been viewed over a million times — Breanne can be seen discussing her experience with what felt like “constant UTIs,” despite “having no reason [she] could think of to have a UTI.” She goes on to explain that cranberry juice and antibiotics, two avenues commonly pursued in the treatment of urinary tract infections, had no impact on the discomfort she was feeling, and actually ended up making her feel worse. It was a struggle to find an answer for what was going on with her body before she was finally told she was living with interstitial cystitis.

Unfortunately, Breanne is not alone in this. According to the National Institutes of Health, it’s estimated that this condition may affect anywhere between 3 million and 8 million women, and between 1 million and 4 million men, in the United States alone.
But because there is a lack of information about this condition, because it sometimes mimics other disorders (like a UTI), and because it primarily affects women, it is often misdiagnosed or missed altogether.
Breanne Rodgers / Via tiktok.com
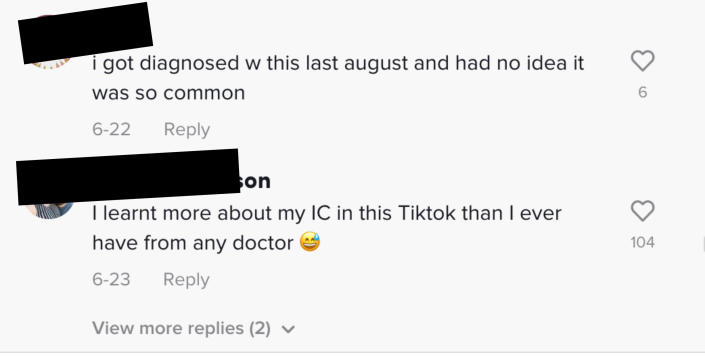
And based on the comments section on Breanne’s TikTok, there’s even more evidence that this is more common than we may think.


BuzzFeed caught up with Breanne to ask her more about her experience, and she told us, “I had been experiencing this incredible pain that disguised itself as a urinary tract infection. Every time I would tell my friends and mom about my symptoms, they would point out how often I was experiencing this and vocalize that they could not relate. I felt so alone and like something must be wrong with me.”

She continued, telling BuzzFeed that she went to the doctor’s office multiple times and was even put on antibiotics for a UTI, which did nothing to squelch the discomfort she was feeling, before finally being diagnosed with interstitial cystitis. “IC is more common than most people realize,” said Breanne, who also said that she believes her video provided some comfort, and even a sense of companionship, to those experiencing IC. She continued, “I know that I spent nearly every night wide awake in bed researching why my bladder was causing me this level of discomfort and/or pain nearly every other day. It truly is a lonely feeling not knowing what is wrong with you or anyone else battling the same issue.”
Breanne Rodgers / Via tiktok.com
In order to get more information about this relatively common but misunderstood condition, we spoke with some experts in the field: Dr. Emily C. Von Bargen, a urogynecologist and medical adviser to vaginal health brand Cheeky Bonsai; Stephanie A. Prendergast, MPT, an all-around expert on pelvic health with the Pelvic Health and Rehabilitation Center; and Krystal Thomas-White, PhD, a senior scientist at vaginal health brand Evvy.

Clockwise from left: Dr. Von Bargen, Stephanie A. Prendergast, and Krystal Thomas-White
Dr. Emily C. Von Bargen, Katelyn Tucker Photography, Krystal Thomas-White
First: What exactly is interstitial cystitis? Also commonly referred to as painful bladder syndrome, this condition is identified most commonly by chronic pelvic pain.

According to Von Bargen, interstitial cystitis, or painful bladder syndrome, can be characterized as “a chronic condition that causes unpleasant sensations attributable to the bladder that have lasted more than six weeks without an identifiable cause.” She continued, telling BuzzFeed, “Bladder symptoms can be described as pain or pressure, discomfort, or spasms. Some of the symptoms can be confused with having a UTI. For example, you might feel the urge to pee all the time or experience painful sex.” And while it has been historically referred to as “interstitial cystitis,” you will also see it commonly referred to as “painful bladder syndrome” these days, and that’s because there is no evidence that the cause of this condition is an actual bladder inflammation (cystitis). Instead, said Von Bargen, patients with symptoms of this condition have a chronic pain condition of the bladder.
Thomas-White emphasized this, explaining that while there are actually a wide range of symptoms, most people who suffer from IC/PBS describe “pain originating in the bladder along with feelings of urinary urgency (the ‘gotta go!’ feeling) and urinary frequency (peeing often).” Thomas-White also noted that If you have ever had a UTI, that feeling is similar to what painful bladder syndrome feels like, except it does not go away with treatment and there is no identifiable infection.
Globalmoments / Getty Images/iStockphoto
And while this condition is not as uncommon as it may seem, diagnosis remains somewhat tricky because, as Thomas-White pointed out to BuzzFeed, interstitial cystitis/painful bladder syndrome is a diagnosis of exclusion. “That means that it doesn’t have a known cause. People diagnosed with IC/PBS must have all other possible diagnoses excluded, from UTIs to cancer. If you don’t fit into one of the medically defined boxes that we know causes pelvic pain, then you get placed into the IC/PBS category.”

However, even though it is a diagnosis of exclusion, the diagnostics used to exclude conditions like UTIs are flawed. Thomas-White goes into more detail about this, explaining to BuzzFeed, “The standard urine culture is the gold standard for diagnosing or excluding UTIs. However, the standard urine culture is biased to culturing a single organism (E. coli) and is really bad at detecting anything else. Research has shown that 20% of women with UTI symptoms are standard culture negative, and standard culture misses up to 50% of all known uropathogens. Therefore, it is quite possible that someone with a diagnosis of IC/PBS has an undiagnosed chronic UTI or … chronic nerve pain [caused by one].” This certainly complicates things.
Javi Sanz / Getty Images/iStockphoto
But in those patients who do appear to have IC/PBS, there are few widely accessible treatment options, and no known cure at this stage. Thomas-White told BuzzFeed that while there has been a lot of research done to try to identify the cause of IC/PBS, the culprit has yet to be found. Bacterial, viral, and fungal infections have all been looked at, and all show some promise, Thomas-White said. But nothing has come up as the obvious cause. Therefore, she added, “It is likely that people living with IC/painful bladder syndrome come about their symptoms in different ways.”
And while there are some treatment options available for this condition, there is still a lot that we don’t know. In her video, Breanne mentioned being put on something that is commonly referred to as the “IC diet.” Oftentimes, people living with this painful condition can find that their pain is made worse with certain “trigger foods,” like coffee, spicy seasonings, and acidic substances (like cranberry juice!) But as with many chronic pain conditions, while there are some avenues of treatment, nothing has been proved to be 100% effective for all patients living with this condition.

Although the “IC diet” isn’t foolproof and doesn’t work the same way for everyone, Breanne was relieved to experience some relief from her own symptoms. “Thanks to the elimination diet my doctor recommended, I now know which foods and drinks I can anticipate causing a flare-up.”
Unfortunately, according to Thomas-White, most patients end up going through a trial-and-error period to try to figure out what works for them. Patients are often counseled to figure out if there are any lifestyle choices that could be triggers, and any food or activities that cause flares. Another step would be to have pelvic floor physical therapy, which could decrease nerve stimulation in the pelvic region and improve symptoms. There are also options for oral or local medications or bladder instillations designed to manage pain, Thomas-White said, noting that “different approaches will be appropriate for different individuals.”
Breanne Rodgers / Via tiktok.com
Stephanie Prendergast often sees IC or painful bladder syndrome in her practice. “The general medical community does not understand this condition. This is a limitation to effective treatment plans. Many patients are told they have an incurable disease by underinformed doctors, and may be handed a ‘one size fits all’ approach of prescription medication and bladder instillations from purported ‘experts.'”

She continued: “I consider IC to fall under the pelvic pain umbrella; this can affect 1 in 3 premenopausal women. Most people need pelvic floor physical therapy, including those who live with IC/painful bladder syndrome, but the physical therapists that specialize in pelvic pain are often out of network/cost prohibitive. There are significant financial barriers to treatment and limited access to informed providers.” However, if you do have access to pelvic floor physical therapy, it can be a great tool to help mitigate symptoms associated with IC/PBS.
Aj_watt / Getty Images
Another reason people continue to suffer, Prendergast said, is that there is no one-size-fits-all approach to management of this condition, and a lack of truly informed doctors and physical therapists is an added barrier to care. She added that she has had tremendous success in her own practice by using critical reasoning and an interdisciplinary network to help her patients resolve their symptoms.
Studies show that over 90% of people with IC also have pelvic floor dysfunction, but, Prendergast said, they need to see a pelvic floor physical therapist skilled in managing pelvic pain. The number of pelvic floor PTs who are available to treat pain is even less than the small number of PTs who can treat other types of pelvic floor dysfunction. Thomas-White added that, unfortunately, like so many aspects of vaginal and urinary health (and most of female healthcare overall!), these conditions are under-researched and broadly defined, which makes effective diagnostics and treatments unattainable for many living with this condition (and others like it).
But despite the barriers and lack of information, experts agree that there is hope and brighter days ahead for people who live with this condition.

Prendergast said she wants people to have hope that this condition can get better. “It is the norm, not the exception, to have issues with various treatments such as medications, physical therapy, procedures, etc. Sometimes things are not tolerated, and sometimes they are simply not effective. The timing and sequence of treatments matter, and if one thing isn’t working or is not tolerated, there are things that can be done to improve outcomes. Creating a treatment plan is a dynamic and evolving process, and it can work with the right team!”
Von Bargen agreed: “Women sometimes struggle to be heard by healthcare providers. If you feel like your symptoms aren’t being taken seriously or your treatment isn’t working, it’s OK to speak up or seek out other opinions.”
Realpeoplegroup / Getty Images/iStockphoto
As for Breanne, she is overwhelmed by all of the love and support she has received since sharing her story on TikTok, telling BuzzFeed, “The response I received from that video made me finally stop feeling alone and scared. Instead, it felt like I was part of a community — a community of strong and resilient women.” And clearly, as seen in the comments, the people of TikTok appreciate this issue being brought to light.
Breanne added, “I will be forever thankful for the support I received, and I hope I can continue to provide that same level of support to women everywhere. I will periodically post updates and check in on my TikTok IC community!”
TikTok / Via tiktok.com