A bad flu year on top of the pandemic could mean trouble for already-stressed hospitals.
As winter looms and hospitals across the U.S. continue to be deluged with severe cases of
The ongoing pandemic, coupled with the looming flu season, could trigger what doctors call a ‘twindemic.’
No precedent exists for a ‘twindemic’
Given the limited spread of influenza in the general U.S. population last year, our research suggests that the U.S. could see a large epidemic of flu this season. Paired with the existing threat of the highly infectious delta variant, this could result in a dangerous combination of infectious diseases, or a “twindemic.”
Models of COVID-19 and other infectious diseases have been at the forefront of predictions about the COVID-19 pandemic, and have often proved to be predictive of cases, hospitalizations and death.
But there are no historical examples of this type of dual and simultaneous epidemics. As a result, traditional epidemiological and statistical methods are not well suited to project what may occur this season. Therefore, models that incorporate the mechanisms of how a virus spreads are better able to make predictions.
We used two separate methods to forecast the potential impact from last year’s decrease in influenza cases on the current 2021-2022 flu season.
In recent research of ours that has not yet been peer-reviewed, we applied a modeling system that simulates an actual population’s interactions at home and work, and in school and neighborhood settings. This model predicts that the U.S. could see a big spike in flu cases this season.
In another preliminary study, we used a traditional infectious disease modeling tool that divides the population into people who are susceptible to infection, those infected, those recovered and those who have been hospitalized or have died. Based on our mathematical model, we predict that the U.S. could see as many as 102,000 additional hospitalizations above the hundreds of thousands that typically occur during flu season. Those numbers assume that there is no change from the usual flu vaccine uptake and effectiveness starting this fall and lasting through the flu season.
Individual behaviors and vaccination matter
A typical flu season usually produces 30 million to 40 million cases of symptomatic disease, between 400,000 and 800,000 hospitalizations and from 20,000 to 50,000 deaths.
This prospect, paired with the ongoing battle against COVID-19, raises the possibility of a twindemic overwhelming the health care system as hospitals and ICUs in some parts of the country overflow with critically ill COVID-19 patients.
Our research also highlighted how young children could be particularly at risk since they have lower exposure to previous seasons of influenza and thus haven’t yet developed broad immunity, compared with adults. In addition to the burden on children, childhood influenza is an important driver of influenza in the elderly as kids pass it on to grandparents and other elderly people.
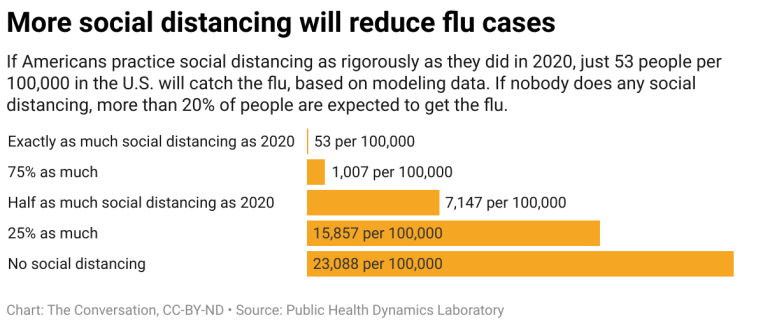
However, there is reason for optimism, since people’s behaviors can change these outcomes considerably.
For instance, our simulation study incorporated people of all ages and found that increasing vaccination among children has the potential to cut infections in children by half. And we found that if only 25% more people than usual are vaccinated against influenza this year, that would be sufficient to reduce the infection rate to normal seasonal influenza levels.
Across the U.S., there is a lot of variability in vaccination rates, adherence to social distancing recommendations, and mask-wearing. So it is likely that the flu season will experience substantial variation state to state, just as we have seen with patterns of COVID-19 infection.
All of this data suggests that although vaccination against influenza is important every year, it is of utmost importance this year to prevent a dramatic rise in influenza cases and to keep U.S. hospitals from becoming overwhelmed.
Written by:
- Mark S Roberts – Distinguished Professor of Health Policy and Management, University of Pittsburgh
- Richard K Zimmerman – Professor of Family Medicine, University of Pittsburgh
This article was first published in The Conversation.